The Complete Guide to Pressure Sores: Causes and Prevention
We hope you find this Nursing Home Neglect Blog Article both Helpful and Informative.
What are pressure sores and how are they caused?
Pressure sores, also known as bedsores or pressure ulcers, are skin injuries that result from prolonged pressure on a particular area of the body. According to the CDC, about 11% of nursing home residents have pressure sores. They commonly occur in regions where the skin covers bony areas, such as heels, hips, and tailbones. These sores occur more in the elderly because nursing homes fail to turn and reposition people who are bedridden, use wheelchairs, or are unable to change positions regularly.
So, how are they caused? The primary factor is continuous pressure on a specific area, which hampers blood flow to the tissues. This lack of blood supply causes the affected tissue to die, leading to the formation of a sore. Friction and moisture can also contribute to the development of pressure sores.
Types of Pressure Sores
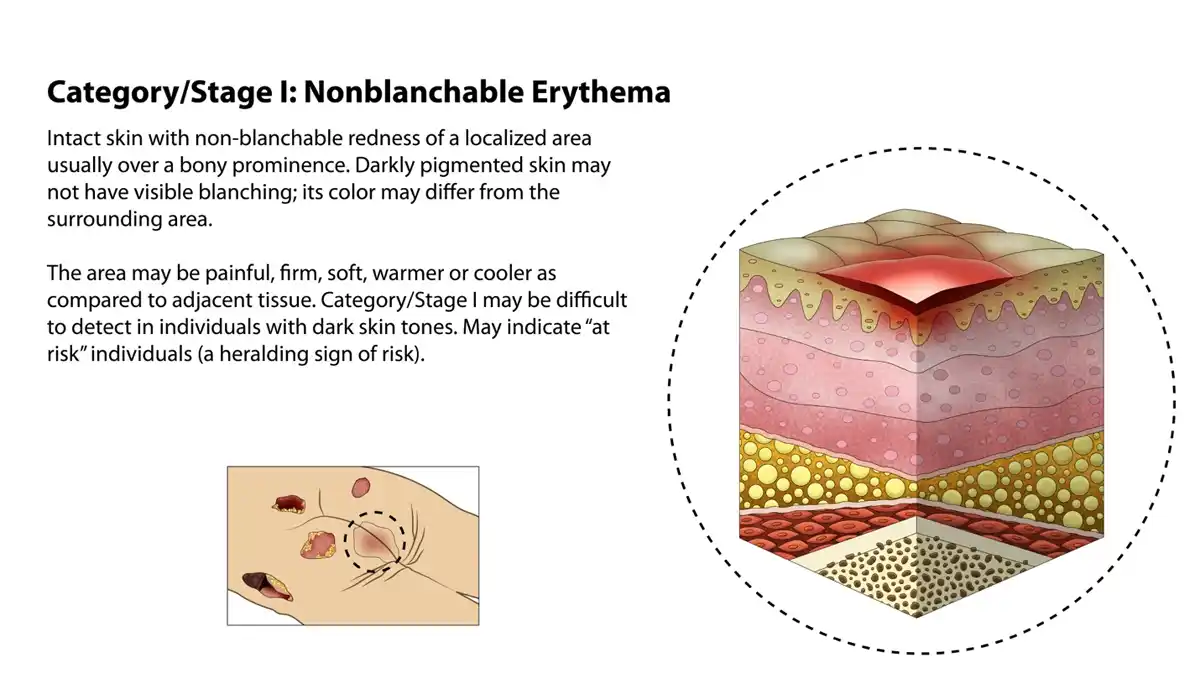
Stage 1
At this stage, the skin is not broken but appears red on individuals with lighter skin tones. A study published in the Journal of Tissue Viability emphasizes the importance of early detection at this stage. For those with darker skin, the affected area may show discoloration. It’s essential to identify and treat pressure sores at this initial stage to prevent further complications.
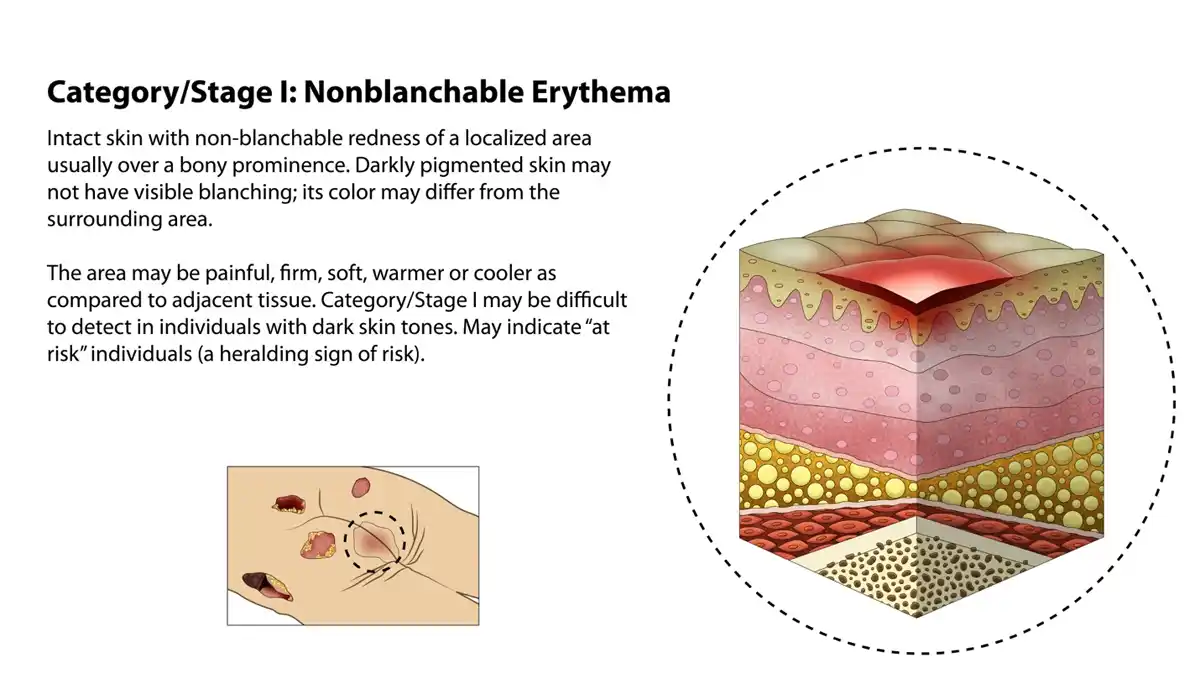
Stage 2
The sore has now progressed to an open ulcer, and the outer layer of the skin is damaged. The wound may resemble a blister filled with clear fluid. At this stage, proper wound care is critical to promote healing.
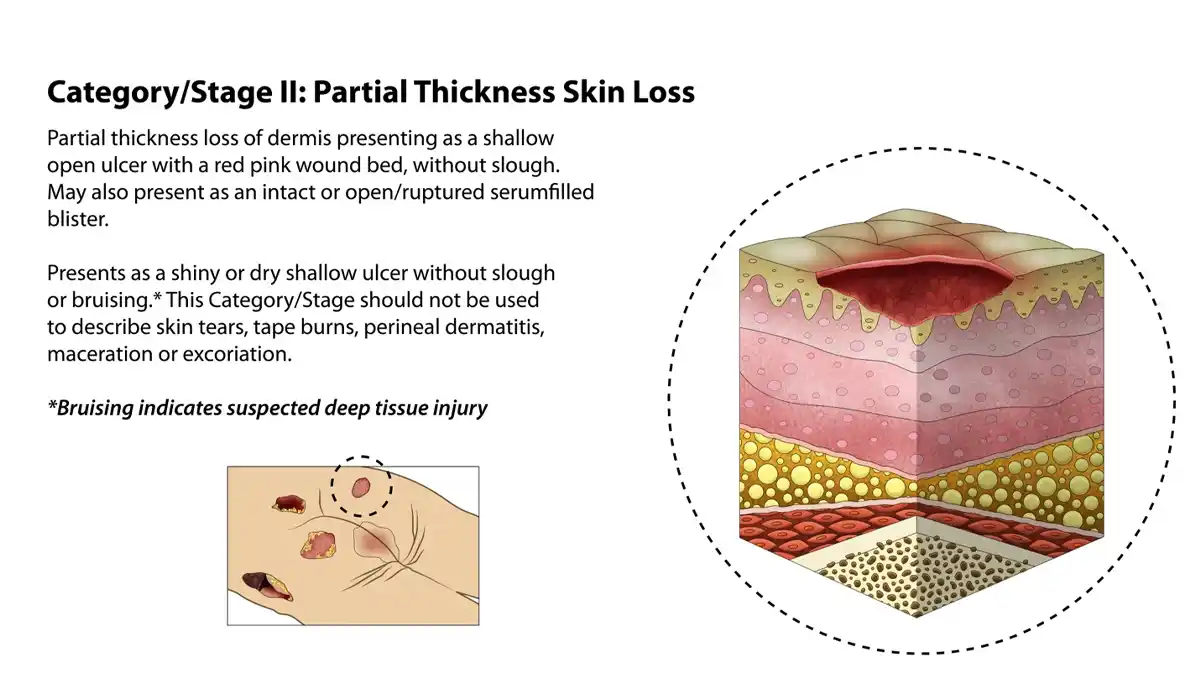
Stage 3
The pressure sore worsens, affecting the layers beneath the skin, extending into the fat layer. The sore appears like a small crater, and bad odors may emanate from the wound due to dead tissue.
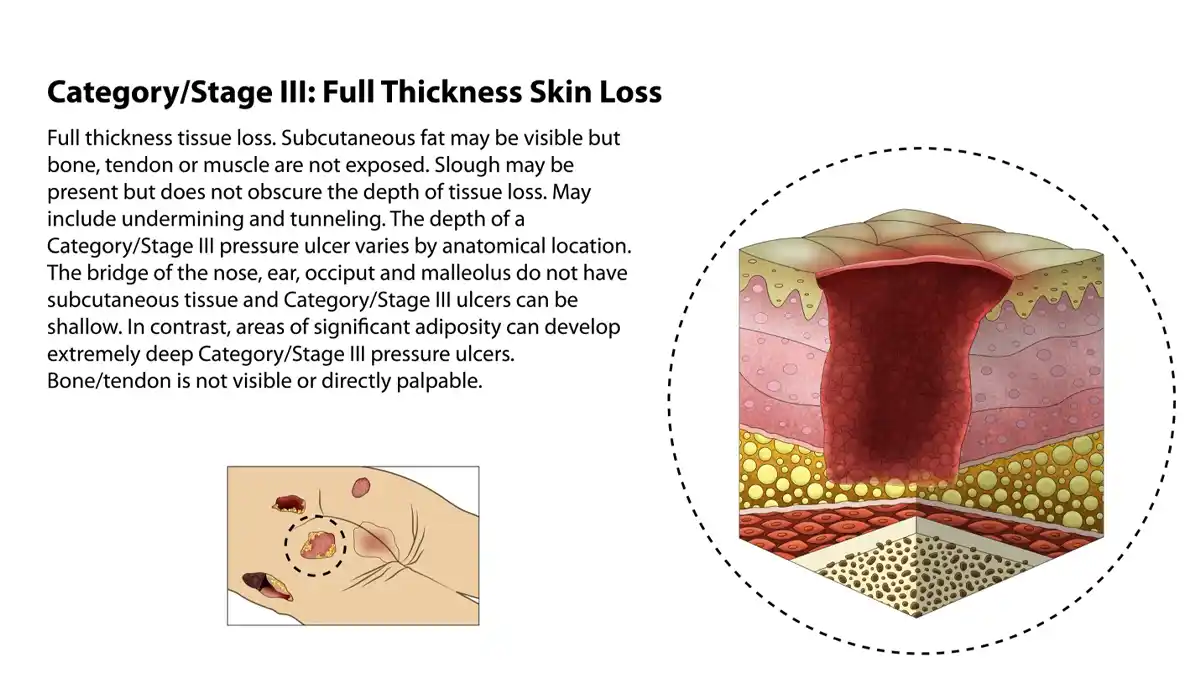
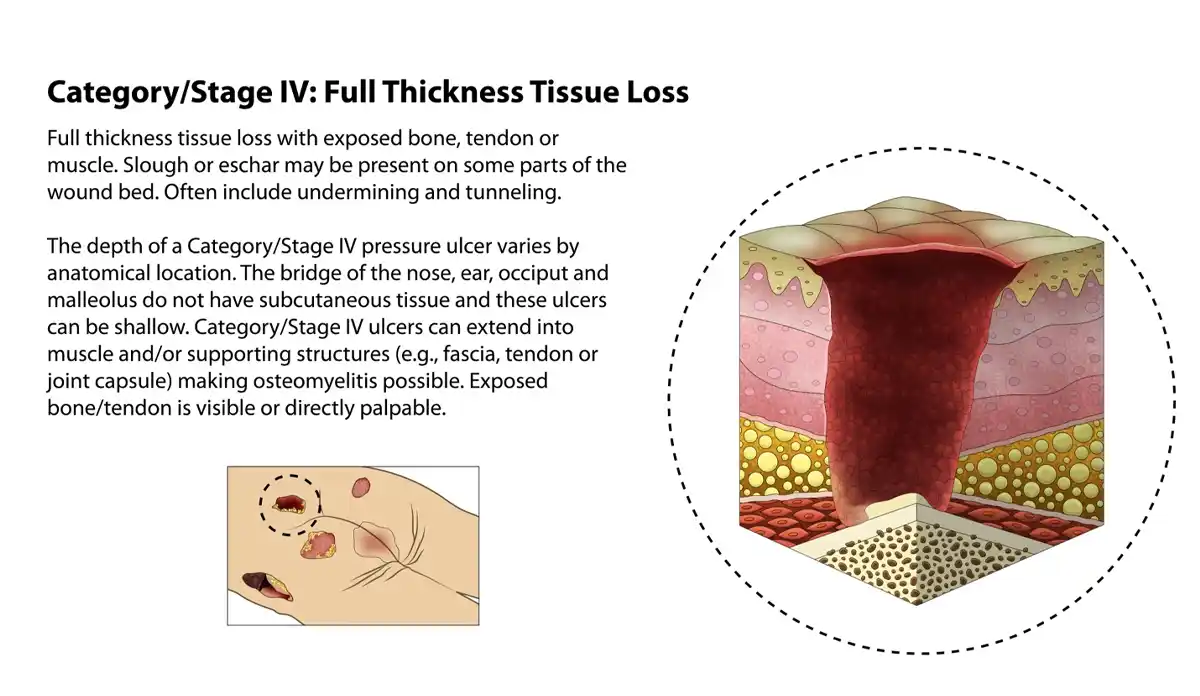
Stage 4
This is the most severe form, where the damage extends to the muscle and even the bone. At this point, the sore is very deep, making it significantly harder to treat.
Causes and Risk Factors
Immobility
The failure of staff, either due to understaffing or neglect, leads to ignoring the needs of many elderly residents to be turned, repositioned, or moved regularly is the chief culprit behind the development of pressure sores. Residents dependent on staff who are confined to a bed or a wheelchair are at heightened risk.
Failure to Use Pressure Reduction Devices
Nursing Homes have the ability to use air mattresses or pressure reduction devices on beds and wheelchairs in order to reduce pressure faced by dependent elderly residents. These devices in many cases can be used without need for a physician’s order. Even if a physician’s order is necessary it is the role of the nursing home to make those recommendations when they assess the resident is at risk for these bedsores.
Poor Nutrition
According to the National Institutes of Health (NIH), inadequate nutrition significantly increases the risk of pressure sores. Malnutrition can make the skin more vulnerable to pressure sores. A diet rich in protein, vitamins, and minerals is crucial for maintaining skin health. If a nursing home fails to provide proper nutrition assessments this can lead to a failure.
Symptoms and Diagnosis
Visual Signs
Redness, discoloration, or open wounds are clear visual indicators of a pressure sore.
Pain Levels
Different stages of pressure sores come with varying levels of pain, ranging from mild discomfort to severe pain.
Complications
Infections
If not treated promptly, pressure sores can lead to skin and even bone infections.
Sepsis
In extreme cases, the bacteria can enter the bloodstream, leading to sepsis, a life-threatening condition.
Prevention Strategies
Regular Movement
According to the National Pressure Ulcer Advisory Panel, regular repositioning can significantly reduce risk. Rotating a person’s position regularly can significantly reduce the risk of developing pressure sores.
Proper Nutrition
A balanced diet is essential for skin health and can go a long way in preventing pressure sores.
Pressure-relieving Devices
Medical-grade cushions and mattresses can be effective preventive measures. A study in the Journal of Clinical Nursing supports this claim. Cushions and mattresses designed to relieve pressure can be highly effective preventive measures.
Regular Skin Checks
Regular skin checks can help identify pressure sores at their earliest stages, making them easier to treat.
Implementing Preventive Measures
Caregivers can significantly reduce the risk by regularly moving the person and maintaining skin hygiene.
Myths and Misconceptions
Pressure Sores are Unavoidable
Many believe that pressure sores are an inevitable part of being bedridden or wheelchair-bound, which is not true.
Only Elderly People Get Them
While more common in older individuals, pressure sores can affect people of all ages.
FAQs
- What are the first signs of a pressure sore?
The first signs usually include redness and discomfort in the affected area. - How long does it take for a pressure sore to heal?
This varies greatly depending on the stage of the sore and the overall health of the individual. - Can pressure sores lead to other medical conditions?
Yes, untreated pressure sores can lead to severe complications like infections and sepsis. - What role do caregivers play in preventing pressure sores?
Caregivers play a pivotal role in both the prevention and management of pressure sores. - What are the best treatment options?
Treatment options range from topical medications to surgical interventions, depending on the severity of the sore.



